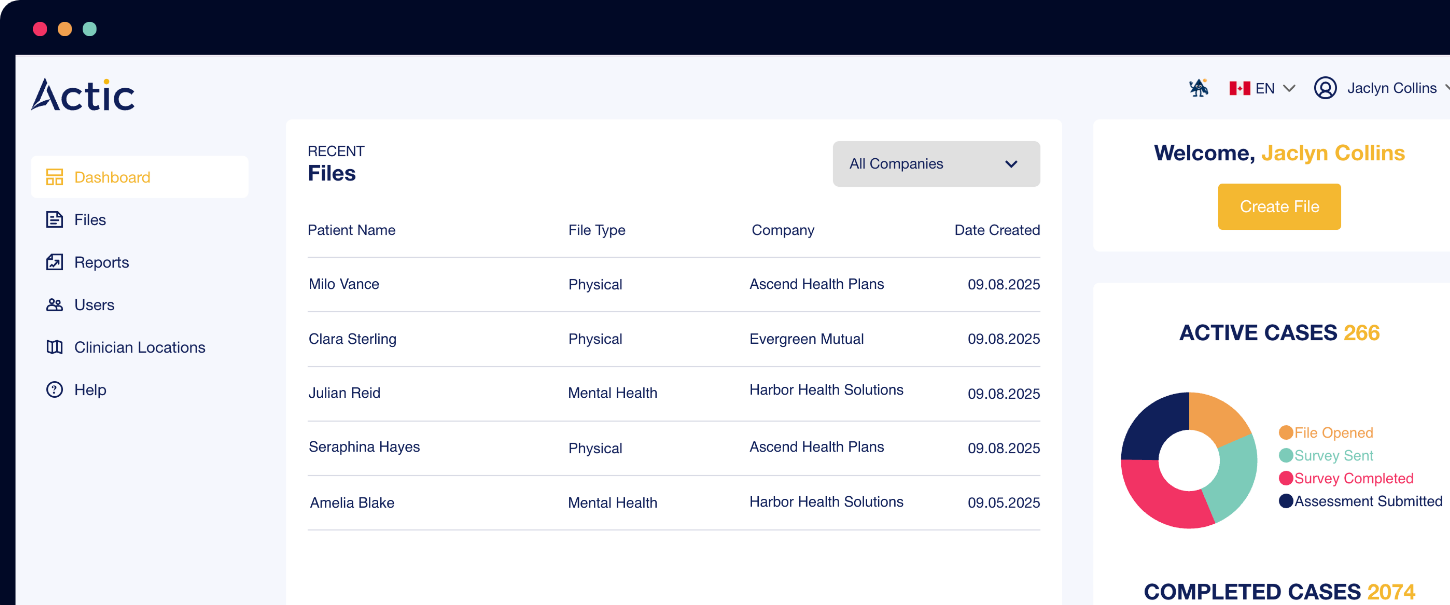












From reducing disability claim durations to providing end-to-end decision intelligence, Actic’s AI-powered platform drives better outcomes, cost savings, and scalable solutions — trusted by Canada’s leading insurers and employers.
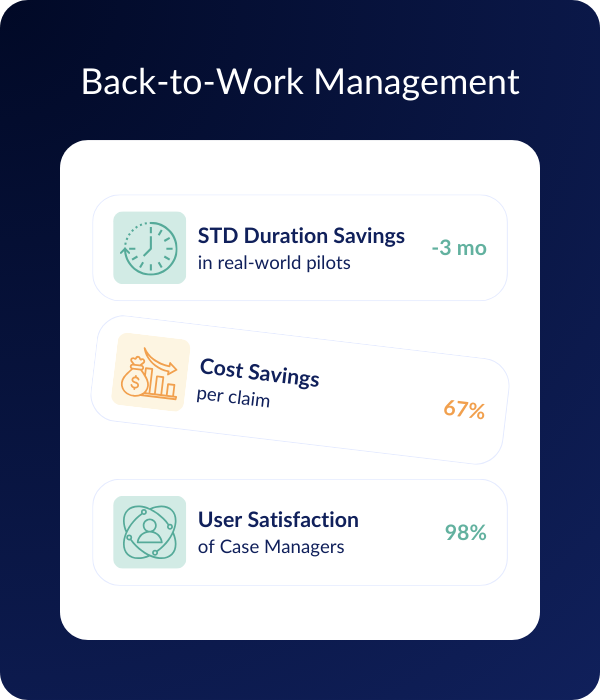
Actic cut Short-Term Disability (STD) duration by 3 months in real-world pilots. Delivered 67% per-claim cost savings and minimal Long-Term Disability (LTD) conversions.
From day one of absence to return-to-work, Actic’s AI tracks care, flags risk, aligns billing, and delivers real-time decision support—end-to-end.
Founded by clinicians and enterprise tech leaders. Deployed with Canada Life, RBC Insurance, Medavie, Equitable Life, and others.
Actic.ai stands at the forefront of revolutionizing employee absence and disability management by offering unparalleled and comprehensive tools aimed at maintaining a resilient workforce. With a keen focus on minimizing absenteeism, improving HR processes, and simplifying worker re-integration, Actic.ai stands out in a market cluttered with fragmented solutions. Our approach directly impacts turnover reduction, mitigates extensive costs associated with employee absenteeism, and significantly eases income replacement obligations for insurers, thereby decreasing year-over-year premium increases for employers.
We give insurers and employers an AI teammate and software that:
From legacy to streamlined results, fuelled by proprietary clinical data and vertical AI.
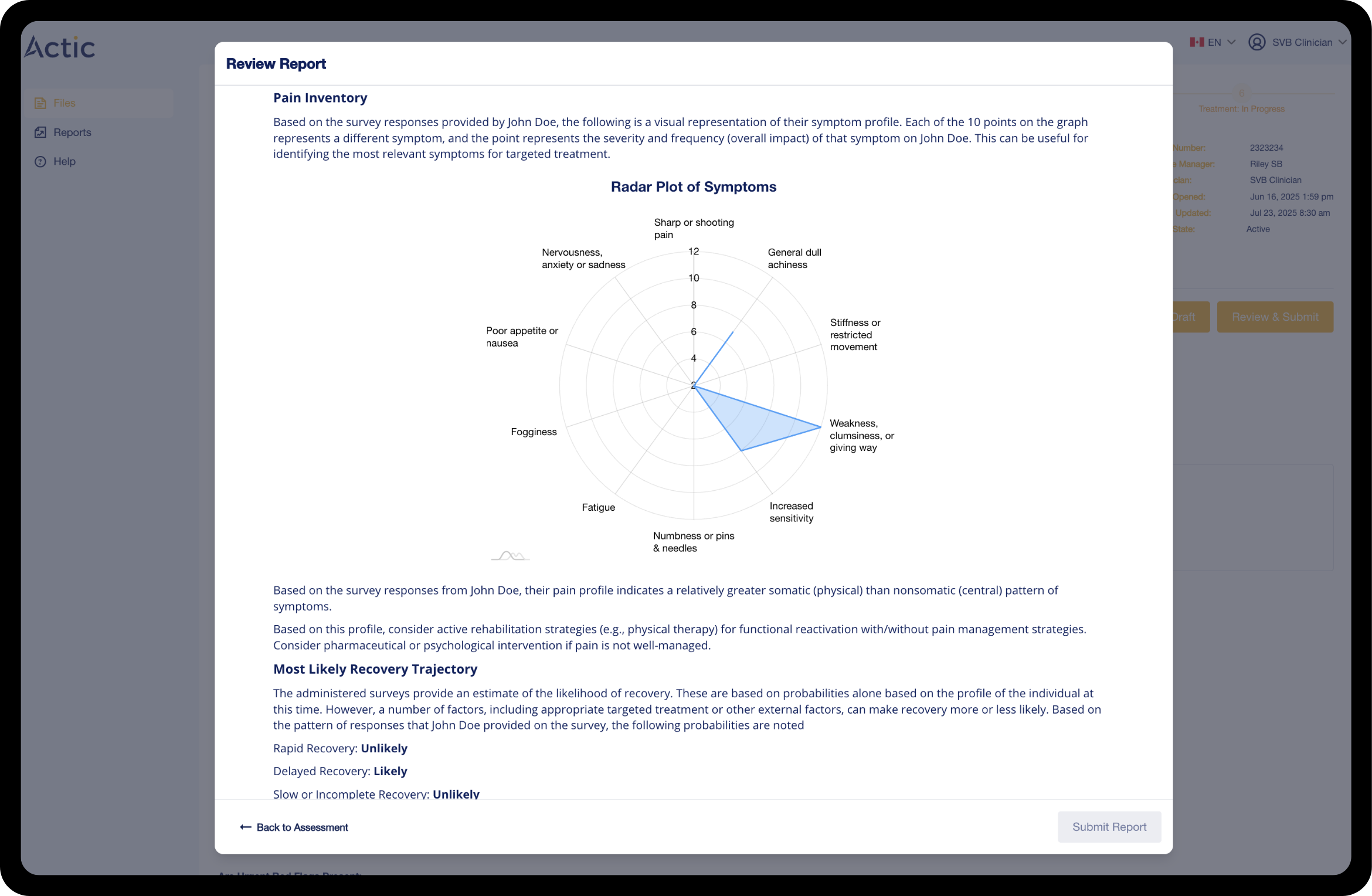
Actic transforms every stage of the claims journey into a seamless, automated process. From instant intake and risk triage to real-time treatment tracking, automated payment audits, and AI-powered return-to-work planning, our platform gives you complete visibility and control. By connecting data, predicting outcomes, and guiding decisions at every step, Actic helps you reduce delays, improve accuracy, and deliver better results for claimants, providers, and employers alike.
Ingest & Triage
Claims are ingested immediately. Risk scoring and triage happen in hours—not weeks.
Understand the Person, Predict the Outcome
With a 360° view of each claimant, accurately forecast recovery timelines, reserves, and risks — transforming uncertainty into clarity.
Real-Time Treatment Tracking
Track every clinical interaction. Flag drift, fraud, or treatment gaps automatically.

Automated Payment + Audits
Link billing directly to care plans. Audit and approve without manual intervention.
Return-to-Work, Reimagined
Our vocational module enables intelligent, AI-powered transferable skills reporting and labour market reviews in a few clicks.
Discover Actic’s suite of intelligent modules designed to simplify claims, improve accuracy, and accelerate recovery.
Make smarter return-to-work decisions faster. Actic’s AI-driven VOC module delivers instant skills reports, personalized retraining options, and real-time job matching — cutting costs by up to 90%.
Actic has delivered measurable cost savings, faster recoveries, and higher satisfaction for national insurers and employers.
Let’s talk about how we can do the same for your team.
Actic’s platform not only drives clinical and financial results — it builds trust and confidence for the people using it.
Join insurers and employers accelerating recovery, reducing costs, and restoring lives—at scale.